Leg Length Discrepancy
Every person?s body is unique and will show different symptoms due to a short leg. Athletes are able to distinguish the negative effects of a leg length that is just 3 mm shorter then the other. A whole host of negative effects can occur to the body that can create chronic pain and may necessitate surgical interventions. The effect of a short leg can be seen almost everywhere in the body.

Causes
Sometimes the cause of LLD is unknown, yet the pattern or combination of conditions is consistent with a certain abnormality. Examples include underdevelopment of the inner or outer side of the leg (hemimelias) or (partial) inhibition of growth of one side of the body of unknown cause (hemihypertrophy). These conditions are present at birth, but the limb length difference may be too small to be detected. As the child grows, the LLD increases and becomes more noticeable. In hemimelia, one of the two bones between the knee and the ankle (tibia or fibula) is abnormally short. There also may be associated foot or knee abnormalities. Hemihypertrophy or hemiatrophy are rare conditions in which there is a difference in length of both the arm and leg on only one side of the body. There may also be a difference between the two sides of the face. Sometimes no cause can be found. This type of limb length is called idiopathic. While there is a cause, it cannot be determined using currect diagnostic methods.
Symptoms
The symptoms of limb deformity can range from a mild difference in the appearance of a leg or arm to major loss of function of the use of an extremity. For instance, you may notice that your child has a significant limp. If there is deformity in the extremity, the patient may develop arthritis as he or she gets older, especially if the lower extremities are involved. Patients often present due to the appearance of the extremity (it looks different from the other side).
Diagnosis
Infants, children or adolescents suspected of having a limb-length condition should receive an evaluation at the first sign of difficulty in using their arms or legs. In many cases, signs are subtle and only noticeable in certain situations, such as when buying clothing or playing sports. Proper initial assessments by qualified pediatric orthopedic providers can reduce the likelihood of long-term complications and increase the likelihood that less invasive management will be effective. In most cases, very mild limb length discrepancies require no formal treatment at all.
Non Surgical Treatment
The most common solution to rectify the difference in your leg lengths is to compensate for the short fall in your shortest leg, thereby making both of your legs structurally the same length. Surgery is a drastic option and extremely rare, mainly because the results are not guaranteed aswell as the risks associated with surgery, not to mention the inconvenience of waiting until your broken bones are healed. Instead, orthopediatrician's will almost always advise on the use of "heel lifts for leg length discrepancy". These are a quick, simple and costs effective solution. They sit under your heel, inside your shoe and elevate your shorter leg by the same amount as the discrepancy. Most heel lifts are adjustable and come in a range of sizes. Such lifts can instantly correct a leg length discrepancy and prevent the cause of associate risks.

Surgical Treatment
Many people undergo surgery for various reasons - arthritis, knee replacement, hip replacement, even back surgery. However, the underlying cause of leg length inequality still remains. So after expensive and painful surgery, follow by time-consuming and painful rehab, the true culprit still remains. Resuming normal activities only continues to place undue stress on the already overloaded side. Sadly so, years down the road more surgeries are recommended for other joints that now endure the excessive forces.
Posterior Tibial Tendon Dysfunction Surgery Prognosis
Overview Posterior tibial tendon insufficiency (also called posterior tibial tendon dysfunction or adult acquired flatfoot) has been named literally after failure of the posterior tibial tendon. However, the condition is caused not only by the progressive failure of the posterior tibial tendon; it is also failure of associated ligaments and joints on the inner side of the ankle and foot. This results in collapse of the arch of the foot, along with the deformity which most often becomes the debilitating problem in its later stages. While at the beginning the common symptom is pain over the tendon in the inner part of the hindfoot and midfoot, later on it is the deformity that can threaten a person?s ability to walk. Just as the tendon degenerates and loses its function, other soft tissue on the same inner side of the foot - namely the ligaments - degenerate and fail. Ligaments are responsible for holding bones in place, and when they fail, bones shift to places where they shouldn?t; deformity is the result. The deformity causes malalignment, leading to more stress and failure of the ligaments.  Causes The cause of posterior tibial tendon insufficiency is not completely understood. The condition commonly does not start from one acute trauma but is a process of gradual degeneration of the soft tissues supporting the medial (inner) side of the foot. It is most often associated with a foot that started out somewhat flat or pronated (rolled inward). This type of foot places more stress on the medial soft tissue structures, which include the posterior tibial tendon and ligaments on the inner side of the foot. Children nearly fully grown can end up with flat feet, the majority of which are no problem. However, if the deformity is severe enough it can cause significant functional limitations at that age and later on if soft tissue failure occurs. Also, young adults with normally aligned feet can acutely injure their posterior tibial tendon from a trauma and not develop deformity. The degenerative condition in patients beyond their twenties is different from the acute injuries in young patients or adolescent deformities, where progression of deformity is likely to occur. Symptoms Symptoms are minor and may go unnoticed, Pain dominates, rather than deformity. Minor swelling may be visible along the course of the tendon. Pain and swelling along the course of the tendon. Visible decrease in arch height. Aduction of the forefoot on rearfoot. Subluxed tali and navicular joints. Deformation at this point is still flexible. Considerable deformity and weakness. Significant pain. Arthritic changes in the tarsal joints. Deformation at this point is rigid. Diagnosis Starting from the knee down, check for any bowing of the tibia. A tibial varum will cause increased medial stress on the foot and ankle. This is essential to consider in surgical planning. Check the gastrocnemius muscle and Achilles complex via a straight and bent knee check for equinus. If the range of motion improves to at least neutral with bent knee testing of the Achilles complex, one may consider a gastrocnemius recession. If the Achilles complex is still tight with bent knee testing, an Achilles lengthening may be necessary. Check the posterior tibial muscle along its entire course. Palpate the muscle and observe the tendon for strength with a plantarflexion and inversion stress test. Check the flexor muscles for strength in order to see if an adequate transfer tendon is available. Check the anterior tibial tendon for size and strength. Non surgical Treatment Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery and progression of your condition can be arrested. In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle, and increasing limitations on walking, running, or other activities. In many cases of PTTD, treatment can begin with non-surgical approaches that may include orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may provide you with an ankle brace or a custom orthotic device that fits into the shoe. Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weight-bearing for a while. Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Shoe modifications. Your foot and ankle surgeon may advise changes to make with your shoes and may provide special inserts designed to improve arch support.
Causes The cause of posterior tibial tendon insufficiency is not completely understood. The condition commonly does not start from one acute trauma but is a process of gradual degeneration of the soft tissues supporting the medial (inner) side of the foot. It is most often associated with a foot that started out somewhat flat or pronated (rolled inward). This type of foot places more stress on the medial soft tissue structures, which include the posterior tibial tendon and ligaments on the inner side of the foot. Children nearly fully grown can end up with flat feet, the majority of which are no problem. However, if the deformity is severe enough it can cause significant functional limitations at that age and later on if soft tissue failure occurs. Also, young adults with normally aligned feet can acutely injure their posterior tibial tendon from a trauma and not develop deformity. The degenerative condition in patients beyond their twenties is different from the acute injuries in young patients or adolescent deformities, where progression of deformity is likely to occur. Symptoms Symptoms are minor and may go unnoticed, Pain dominates, rather than deformity. Minor swelling may be visible along the course of the tendon. Pain and swelling along the course of the tendon. Visible decrease in arch height. Aduction of the forefoot on rearfoot. Subluxed tali and navicular joints. Deformation at this point is still flexible. Considerable deformity and weakness. Significant pain. Arthritic changes in the tarsal joints. Deformation at this point is rigid. Diagnosis Starting from the knee down, check for any bowing of the tibia. A tibial varum will cause increased medial stress on the foot and ankle. This is essential to consider in surgical planning. Check the gastrocnemius muscle and Achilles complex via a straight and bent knee check for equinus. If the range of motion improves to at least neutral with bent knee testing of the Achilles complex, one may consider a gastrocnemius recession. If the Achilles complex is still tight with bent knee testing, an Achilles lengthening may be necessary. Check the posterior tibial muscle along its entire course. Palpate the muscle and observe the tendon for strength with a plantarflexion and inversion stress test. Check the flexor muscles for strength in order to see if an adequate transfer tendon is available. Check the anterior tibial tendon for size and strength. Non surgical Treatment Because of the progressive nature of PTTD, early treatment is advised. If treated early enough, your symptoms may resolve without the need for surgery and progression of your condition can be arrested. In contrast, untreated PTTD could leave you with an extremely flat foot, painful arthritis in the foot and ankle, and increasing limitations on walking, running, or other activities. In many cases of PTTD, treatment can begin with non-surgical approaches that may include orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may provide you with an ankle brace or a custom orthotic device that fits into the shoe. Immobilization. Sometimes a short-leg cast or boot is worn to immobilize the foot and allow the tendon to heal, or you may need to completely avoid all weight-bearing for a while. Physical therapy. Ultrasound therapy and exercises may help rehabilitate the tendon and muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Shoe modifications. Your foot and ankle surgeon may advise changes to make with your shoes and may provide special inserts designed to improve arch support. 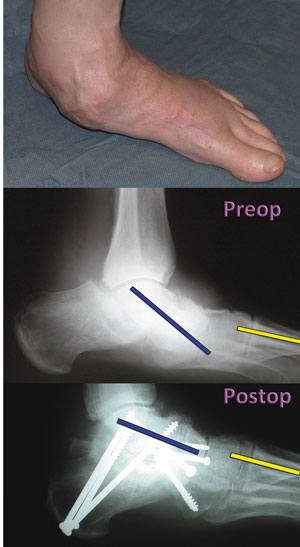 Surgical Treatment Until recently, operative treatment was indicated for most patients with stage 2 deformities. However, with the use of potentially effective nonoperative management , operative treatment is now indicated for those patients that have failed nonoperative management. The principles of operative treatment of stage 2 deformities include transferring another tendon to help serve the role of the dysfunctional posterior tibial tendon (usually the flexor hallucis longus is transferred). Restoring the shape and alignment of the foot. This moves the weight bearing axis back to the center of the ankle. Changing the shape of the foot can be achieved by one or more of the following procedures. Cutting the heel bone and shifting it to the inside (Medializing calcaneal osteotomy). Lateral column lengthening restores the arch and overall alignment of the foot. Medial column stabilization. This stiffens the ray of the big toe to better support the arch. Lengthening of the Achilles tendon or Gastrocnemius. This will allow the ankle to move adequately once the alignment of the foot is corrected. Stage 3 acquired adult flatfoot deformity is treated operatively with a hindfoot fusion (arthrodesis). This is done with either a double or triple arthrodesis - fusion of two or three of the joints in hindfoot through which the deformity occurs. It is important when a hindfoot arthrodesis is performed that it be done in such a way that the underlying foot deformity is corrected first. Simply fusing the hindfoot joints in place is no longer acceptable.
Surgical Treatment Until recently, operative treatment was indicated for most patients with stage 2 deformities. However, with the use of potentially effective nonoperative management , operative treatment is now indicated for those patients that have failed nonoperative management. The principles of operative treatment of stage 2 deformities include transferring another tendon to help serve the role of the dysfunctional posterior tibial tendon (usually the flexor hallucis longus is transferred). Restoring the shape and alignment of the foot. This moves the weight bearing axis back to the center of the ankle. Changing the shape of the foot can be achieved by one or more of the following procedures. Cutting the heel bone and shifting it to the inside (Medializing calcaneal osteotomy). Lateral column lengthening restores the arch and overall alignment of the foot. Medial column stabilization. This stiffens the ray of the big toe to better support the arch. Lengthening of the Achilles tendon or Gastrocnemius. This will allow the ankle to move adequately once the alignment of the foot is corrected. Stage 3 acquired adult flatfoot deformity is treated operatively with a hindfoot fusion (arthrodesis). This is done with either a double or triple arthrodesis - fusion of two or three of the joints in hindfoot through which the deformity occurs. It is important when a hindfoot arthrodesis is performed that it be done in such a way that the underlying foot deformity is corrected first. Simply fusing the hindfoot joints in place is no longer acceptable.